Osteoarthritis (OA) is the most common musculoskeletal condition in older people and poses a large burden to the health and social care system. OA can develop in any joint in the body, but when it affects the knee or hip, mobility can be affected leading to disability.
Over 6.5 million people have sought treatment from their GP for OA of the hip and knee. Almost all (98%) of initial knee replacements are due to osteoarthritis.
There are several risk factors for the development of OA, including increasing age, gender, genetic factors, and previous joint injury. The largest modifiable risk factor is obesity.
Given the projected increases in obesity, and the growth and ageing of the population, the proportion of people affected by OA is expected to rise.

Data from Arthritis Research UK estimates that a total of 28,133 people aged 45 or over in Wigan live with knee osteoarthritis. This means that of the total Wigan population aged 45 years or over, 20.2% are estimated to have knee osteoarthritis (overall prevalence).
This is higher than the overall prevalence for England as a whole – 18.2%. Of the total number of people with knee osteoarthritis, 12,478 are male (male prevalence 18.4%) and 15,655 are female (female prevalence 21.8%).
It is estimated that there are 9,990 people with severe knee osteoarthritis, which is 7.2% of the population aged 45 years or over. It is also estimated that a total of 16,416 people aged 45 or over in Wigan live with hip osteoarthritis.
This means that of the total Wigan population aged 45 years or over, 11.8% are estimated to have hip osteoarthritis (overall prevalence). This is higher than the overall England prevalence of 10.9%.
Of the total number of people with hip osteoarthritis, 5,900 are male (male prevalence 8.7%) and 10,516 are female (female prevalence 14.7%). It is estimated that there are 5,106 people in Wigan with severe hip osteoarthritis, which is 3.7% of the population aged 45 years or over.
The cost of hip and knee replacements throughout the borough is approximately £4.5 million a year.
Traditionally within Wigan, we have worked closely with clinical teams within secondary care.
Across all Be Well programmes in 2022, 21% of all referrals reported Musculo-skeletal as a condition.
On the long-term condition programme, we had a total of 2,074 referrals (2022), of which 765 (37%) identified MSK (pain/Injury) and 489 (24%) identified arthritis as their primary medical condition. 225 (11%) had both on their medical history.
Analysis of these 1,029 unique referrals, shows 783 had a first contact with the Be Well team, of these 191 did not take up the pain management pathway programme. Of the 592 that did engage, 450 (76%) completed the programme.
In Sept 22 we started to look at a more proactive approach and look to engage with residents earlier on and prevent them entering the pain/medication cycle.
We wanted to place ourselves at the front end of pain management and identify first instances of pain. NICE makes recommendations about the diagnosis, treatment, and care of people with osteoarthritis. These recommendations include holistic assessment of people with osteoarthritis and core treatments which include activity and exercise, and weight loss if the person is overweight or obese.
We wanted to embed Be Well into this holistic assessment.
We saw the role of the First Contact Practitioners/Physiotherapists (FCPs) as an ideal opportunity to change the way we tackled this issue and the perfect enablers.
The vast majority of musculoskeletal FCPs are physiotherapists with enhanced skills. They can help patients with musculoskeletal issues such as back, neck and joint pain by:
Patients with back and joint pain, including conditions such as arthritis, can contact their local physiotherapist directly, rather than waiting to see a GP or being referred to hospital.
The delivery model was designed to align the FCP leads with Be Well Wellbeing specialist instructors across the seven PCNs. Referrals were assigned directly to the WSI from the FCP and contacted in a timely manner.
The teams have been meeting at our leisure centre sites to visit classes and see facilities, with the aim for the clinical team to be based on within Be Well facilities.
We utilised our wider Be Well physical/nutritional opportunities to support participants including our strength and balance/weight management programme/leisure offer.
More specifically we delivered the ESCAPE Pain Programme (EP), an education and exercise intervention within our leisure centres. This is a six-week intervention for people with knee and hip OA, which Wigan has a higher rate of than other GM areas.
Delivered in 12 sessions, twice weekly, it incorporates a progressive exercise circuit (40 min) and an educational component (usually the last 15-20 mins). The aim of the programme is to reduce pain in the joints and increase mobility and function.
We wanted to evaluate lifestyle factors such as mental health and physical inactivity and more importantly its impact on musculoskeletal health with specific questionnaires (HOOs and KOOS).
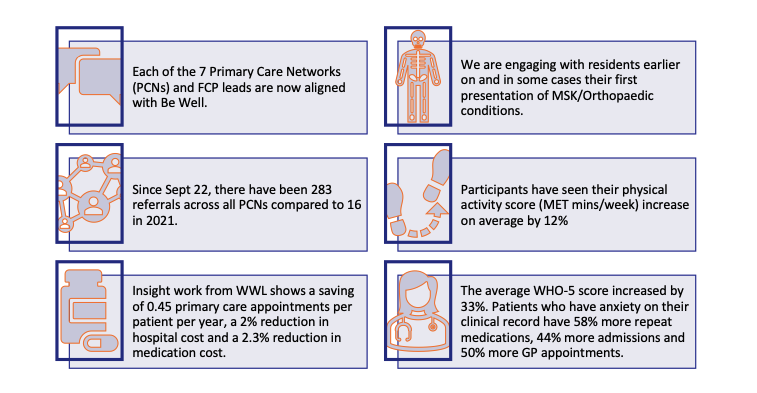
The infographic below highlights the impact since starting the new pathway in Sept 22. Including increasing physical activity levels (IPAQ – a physical activity questionnaire looking at vigorous, moderate, walking) and improvements in mental health score (WHO-5).
We mentioned the Escape Pain earlier in our model and we deliver 5/6 cohorts per year at two sites across the borough: Robin Park Sports Centre and Leigh Leisure Centre (10-12 per year).
We have had 305 attendances at our EP cohorts since the start of our work with the FCPs (Sept 22).
We collected pre and post outcome questionnaires for specific OA measures, HOOS (Hip dysfunction and Osteoarthritis Outcome Score) and KOOS (Knee injury and Osteoarthritis Outcome Score) to determine if a participant has decreased pain and increased function and mobility. The higher the score the more improvements that have been made.
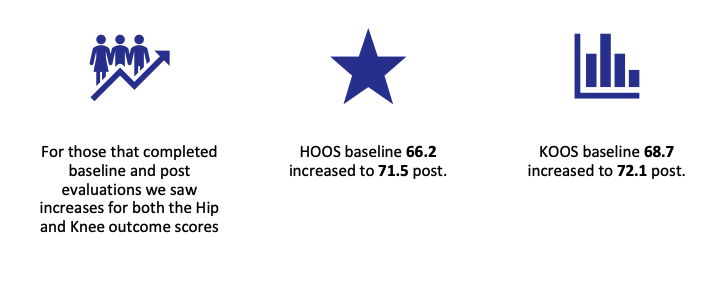
This coupled with the increased IPAQ scores from the infographic suggest a significant impact on the participants. Often introducing PA to those with hip/knee pain and dysfunction can lead to a short-term increase/worsening of symptoms.
A functional test (30 second sit to stand test) testing leg strength and endurance was completed at baseline and post cohort. The average score increased from 9.5 to 13.5, a 42% increase in functional capacity.
Since the scheme was implemented, Be Well has seen great results and stories from people like Roy – benefiting from the range of choices now available to them:
Ideas and projects are continuously evolving and progressing at GM Active. View our latest news stories below to find out how we are moving as one and contributing towards building the healthy, happy and prosperous Greater Manchester we all aspire to.